
Michelle McKenzie explores our guts connection to health and how we can build our inner strength through our food.
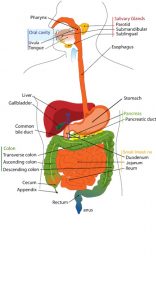 Our gut is fascinating. It’s a complex system that starts in our mouth and is made up of various parts of the body involved in the digestion process such as the oesophagus, gallbladder, liver, stomach, pancreas, duodenum, large intestine, jejunum, appendix, ileum, rectum and anus.
Our gut is fascinating. It’s a complex system that starts in our mouth and is made up of various parts of the body involved in the digestion process such as the oesophagus, gallbladder, liver, stomach, pancreas, duodenum, large intestine, jejunum, appendix, ileum, rectum and anus.
As well as processing food and nutrients and excreting waste, a whopping 80% of our immune system is housed there. 90% of the bodies’ serotonin is produced there and it is home to 100-trillion micro-organisms (mostly bacteria but also a mix of viruses, fungi and protozoa).
These micro-organisms are collectively referred to as the microbiome and weigh 3-5 Ibs in weight, almost the same as the human brain. They interact with the body, with the food we eat and with each other. The gut is now reverently described as ‘our second brain’ and the ‘gateway to health’. Hippocrates who is often referred to as the ‘father of medicine’ had a theory more than 2000 years ago that “all disease begins in the gut”. It looks like he may have stumbled on something!
 Allergies, skin conditions, digestive system disorders (IBS), inflammatory bowel diseases (crohn’s, ulcerative colitis) and autoimmunity are all on the rise and despite not appearing to be related, individuals with autoimmune diseases such as type 1 diabetes, lupus and rheumatic arthritis are reported to have imbalances in their gut microbiome which has potentially triggered these conditions. Research also suggests that metabolic conditions such as type 2 diabetes and obesity are also influenced by the health of our microbiome.
Allergies, skin conditions, digestive system disorders (IBS), inflammatory bowel diseases (crohn’s, ulcerative colitis) and autoimmunity are all on the rise and despite not appearing to be related, individuals with autoimmune diseases such as type 1 diabetes, lupus and rheumatic arthritis are reported to have imbalances in their gut microbiome which has potentially triggered these conditions. Research also suggests that metabolic conditions such as type 2 diabetes and obesity are also influenced by the health of our microbiome.
 Depression and anxiety are also widespread and it is proposed that when the gut becomes compromised and inflamed, this inflammation can trigger changes in our mood due to a direct line of communication between the digestive system and the brain; also known as the gut-brain axis.
Depression and anxiety are also widespread and it is proposed that when the gut becomes compromised and inflamed, this inflammation can trigger changes in our mood due to a direct line of communication between the digestive system and the brain; also known as the gut-brain axis.
The vagus nerve is one of the most important highways in the gut-brain axis, a two-way superhighway delivering sensory information via the nervous system about how we are feeling. This feedback loop is constantly assessing if you are safe or in danger, ‘fight or flight’ or ‘rest and digest’.
Have you have ever experienced that gut feeling or had butterflies in your stomach due to a stressful situation? Research is still ongoing, but there are numerous studies suggesting that supplementing with certain probiotics, can help reduce inflammation and improve anxiety and depression. This provides evidence that our gut bacteria can indeed affect our mood but it also raises the question, could looking after your gut actually prevent depression in the first place?
 There are a number of factors that influence the overall health and population of our microbiome and it starts from the moment we are born. If we have a natural birth, our first encounter with healthy bacteria is in the birth canal, followed by breast feeding. This exposure provides protection and plays an important role in the development of our immune system.
There are a number of factors that influence the overall health and population of our microbiome and it starts from the moment we are born. If we have a natural birth, our first encounter with healthy bacteria is in the birth canal, followed by breast feeding. This exposure provides protection and plays an important role in the development of our immune system.
As we age, factors that can be detrimental to a healthy microbiome include antibiotic use, prescription and recreational drug use, the overuse of antibacterial cleaning products, stress, alcohol intake, exposure to toxins, lack of sleep and what we eat.
 The survival and health of our beneficial probiotic bacteria is heavily influenced by our diet, with specific foods affecting different types of bacteria. It’s probably no surprise that the foods that disrupt the microbiome are foods that have been processed.
The survival and health of our beneficial probiotic bacteria is heavily influenced by our diet, with specific foods affecting different types of bacteria. It’s probably no surprise that the foods that disrupt the microbiome are foods that have been processed.
Processed foods are high in sugar, contain artificial sweeteners, refined seed oils, additives, emulsifiers, pesticides, GMO’s and antibiotic residues that have been used in food production (though ‘seemingly’ more evidence is required regarding the impact of antibiotic residues on our heath).
Diversity is important in both the food we eat and the microbes we feed, so aim to incorporate a wide variety of ‘real’ foods, prebiotic fibre and probiotic bacteria. The microbiome thrive on foods rich in prebiotic fibres (undigestible plant fibres).
Rich sources of these (fructooligosaccharides and inulin) can be found in various amounts in raw asparagus, Jerusalem artichokes, raw chicory root, raw dandelion greens, raw and cooked onions, raw  leeks, raw garlic, raw wheat bran and green bananas. Other types of prebiotic fibre (galactooligosaccharides) can be found in legumes, black beans, kidney beans and chickpeas, cold potatoes (resistant starches), mushrooms, oats (beta-glucans) and apples (pectin).
leeks, raw garlic, raw wheat bran and green bananas. Other types of prebiotic fibre (galactooligosaccharides) can be found in legumes, black beans, kidney beans and chickpeas, cold potatoes (resistant starches), mushrooms, oats (beta-glucans) and apples (pectin).
When the bacteria break down these fibres, they produce butyrate, a short-chain fatty acid that looks after the villi in the gut, enabling growth and stability. Butyrate also helps by looking after the cells that line the gut, by providing energy for the cells, suppressing inflammation, modulating the immune system and playing a role in releasing hunger suppressing hormones and therefore weight loss. Aside from our clever gut flora producing butyrate, dietary sources include butter and full fat dairy. Lightly steamed asparagus with butter anyone?
 As well as feeding the bacteria, it’s important to include foods that are rich in probiotics to help keep populations intact and to ensure that the percentage of good bacteria outweigh the ‘bad’ pathogenic bacteria.
As well as feeding the bacteria, it’s important to include foods that are rich in probiotics to help keep populations intact and to ensure that the percentage of good bacteria outweigh the ‘bad’ pathogenic bacteria.
Probiotics are live micro-organisms that are created through the process of fermentation (which is also one of the oldest ways of preserving food). Rich sources of probiotic bacteria can be found in yogurt, kefir, aged cheeses, fermented live miso, kombucha, fermented vegetables (kimchi, sauerkraut) and tempeh. Probiotic supplements are also widely available with the beneficial effects dependent on the type and strain.
Recent research suggests, that variations of gut microbiota between people could explain why following a low-fat diet versus a high fat diet, or a high carbohydrate versus a low carbohydrate diet, may be beneficial for some but not for others. For optimal health, it may be a case of tailoring diets to suit your personal gut microbiome. As a rule of thumb, I advise clients to eat a diverse, real food diet, rich in plants, low glycaemic fruits (berries and cherries), quality protein and healthy fats (including omega-3) and to avoid foods that are known to cause inflammation and disrupt the microbiome, such as heavily processed seed oils and sugar. This type of diet will also be rich in polyphenols, which promote the growth of beneficial bacteria and antioxidants which will help lower gut inflammation.
and disrupt the microbiome, such as heavily processed seed oils and sugar. This type of diet will also be rich in polyphenols, which promote the growth of beneficial bacteria and antioxidants which will help lower gut inflammation.
Another excellent choice for gut health is bone broth. It’s a source of collagen, proline, gelatine and glutamine which can help repair and maintain a healthy intestinal lining. It is also reported to help with joint pain, support the immune system, aid bone health and help reduce inflammation. It’s best to make it from organic sources and to have it regularly.
Research also indicates that time restricted eating and intermittent fasting can help restore microbe diversity, increase tolerance against ‘bad’ bacteria and restore the integrity of the intestinal epithelium. Intermittent fasting could further promote the impact of a good diet by not only priming our microbes but giving our guts a much -needed rest (and digest). Recent research implies that for maximum health benefits, it’s not only what we eat, but when we eat.
 The good news is that gut bacteria are really responsive to changes in the diet, with a study reporting that within a matter of days there was a greater diversity in the microbiome. Variety appears to be key so follow a real food diet with lots of vegetables, low GI fruit (berries), healthy fat, quality protein, prebiotic fibre (asparagus, leeks) probiotic bacteria (full fat yogurt, cheese) and a daily cup of bone broth. Try and reduce your stress levels, enjoy an occasional glass of red wine, reduce exposure to toxins (smoking, pesticides, GMO foods, household cleaning products), only take antibiotics when really necessary, cut out processed foods and sugar and get your hands dirty in the garden.
The good news is that gut bacteria are really responsive to changes in the diet, with a study reporting that within a matter of days there was a greater diversity in the microbiome. Variety appears to be key so follow a real food diet with lots of vegetables, low GI fruit (berries), healthy fat, quality protein, prebiotic fibre (asparagus, leeks) probiotic bacteria (full fat yogurt, cheese) and a daily cup of bone broth. Try and reduce your stress levels, enjoy an occasional glass of red wine, reduce exposure to toxins (smoking, pesticides, GMO foods, household cleaning products), only take antibiotics when really necessary, cut out processed foods and sugar and get your hands dirty in the garden.
To quote Tim Spector, a leading researcher in gut health “treat our microbiome like a garden – we need to nourish the soil (intestines) for healthy plants (bacteria), while minimising weeds (disease-causing microbes.) “



